Manage your claims directly from your LIS
Laboratory information systems have traditionally handled only the management and operations associated with the laboratory, and other disparate systems handled other operations. With LIS ABC for Toxicology we wanted to develop a tool that would integrate everything in a requisition-centric fashion from physician, with the client web portal, to laboratory operations to medical billing and coding; a fully integrated practice management solution.
All the information you need is now in your LIS system from demographics and insurance to tests ordered - why go to a separate system to generate claims and send to a clearinghouse? As part of our Integrated Practice Management solution, physicians’ offices create new requisitions on a shared screen, so you can immediately review them and add missing information, upload scanned documents, and take pictures of insurance cards to store all of the required information with the requisition. At the end of the process, the final report is approved and sent to the client, and a claim is automatically generated based on tests ordered and insurance carrier information.
Tools to Enable Medical Billing and Coding from LIS ABC
If the physician’s office enters insurance information by scanning an insurance card rather than entering data manually, no problem. When developing the claim process, we added image recognition to pull the readable text right off of the card. This enables you to reduce manual data entry and only requires your billing staff to verify that the information is correct and to update it as needed.
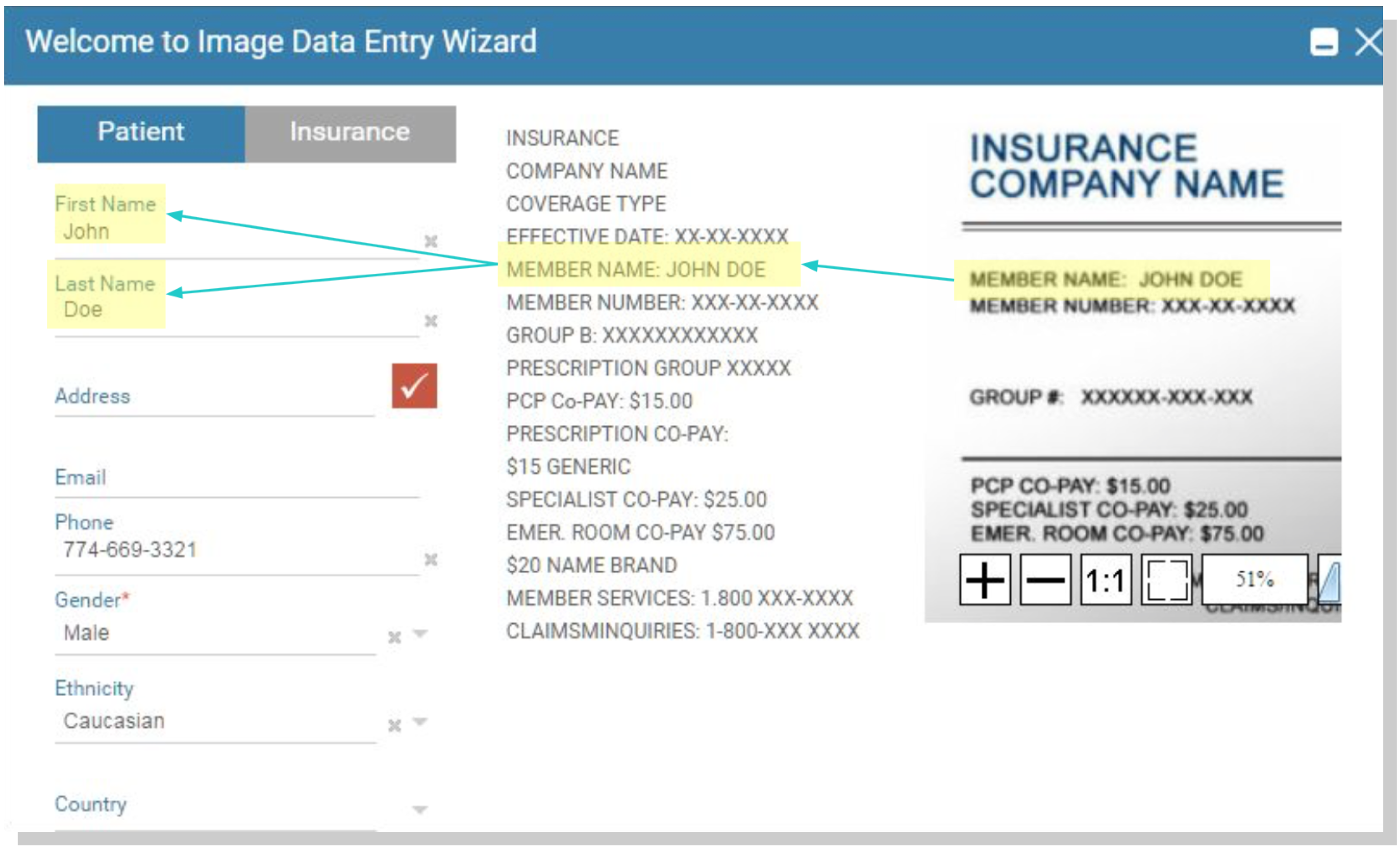
Enter data directly from an Insurance Card with Image Analysis Tools
Furthermore, we made checking insurance benefits much easier by integrating them into LIS ABC, so you aren’t required to go to a separate system to check a patient’s benefits, plan, deductible, and deductible paid. It’s all right there at your fingertips.
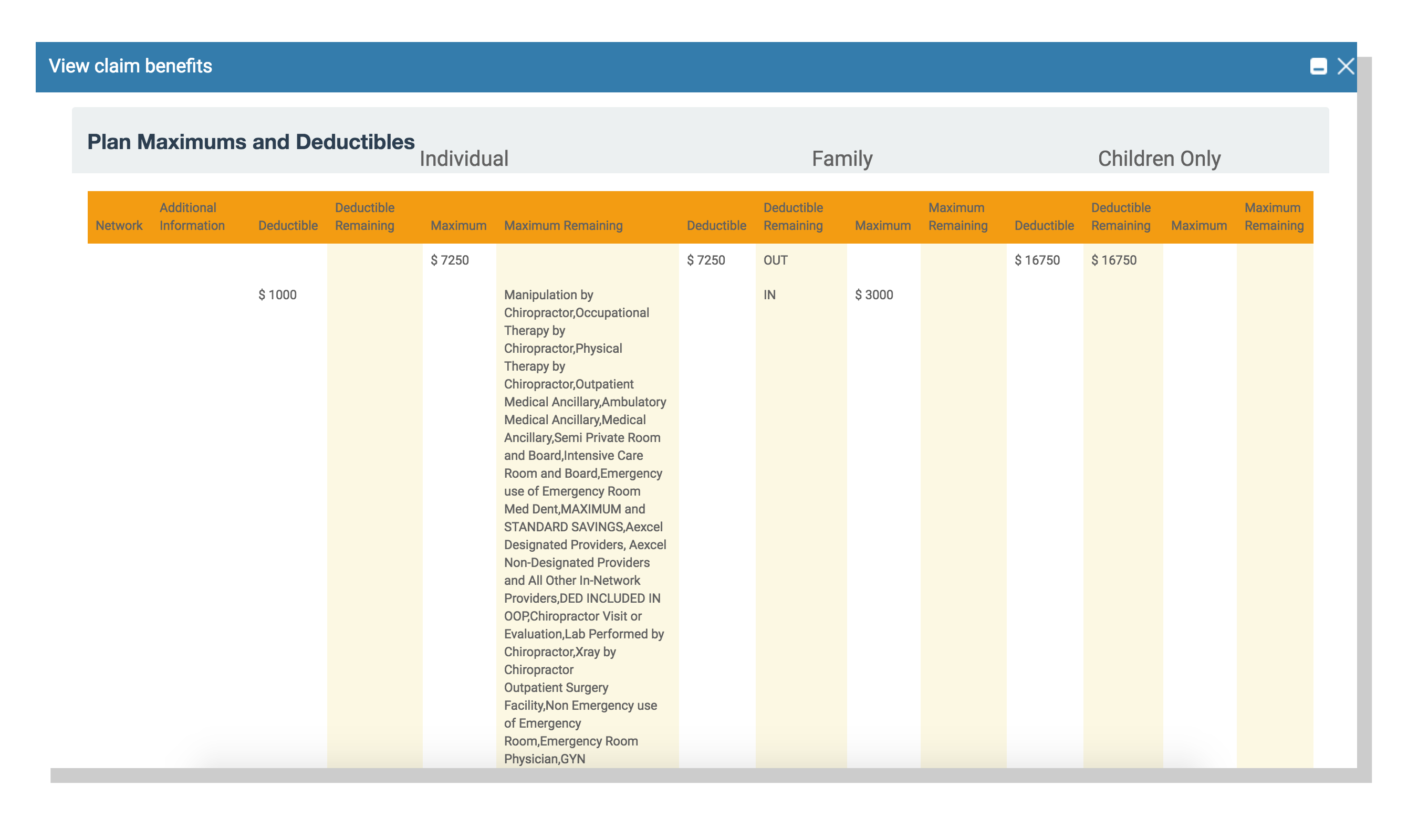
Check Patient Benefit Information Directly from LIS ABC
Now you have all the tools you need to work the claim, including an approval workflow to ensure the proper steps are taken before you submit it to the clearinghouse.You can work the claim through the claim manager; make any necessary adjustments, scrub the claim, track outstanding balances and insurance and patient responsibilities, and keep track of what has already been paid as well as any writeoffs. We also support sending and receiving of electronic 837 and 835 forms.
Published: 6 Apr 2024